✨ Back Health Uncovered: Understanding the Prevention and Diagnosis of Lumbar Disc Herniation✨
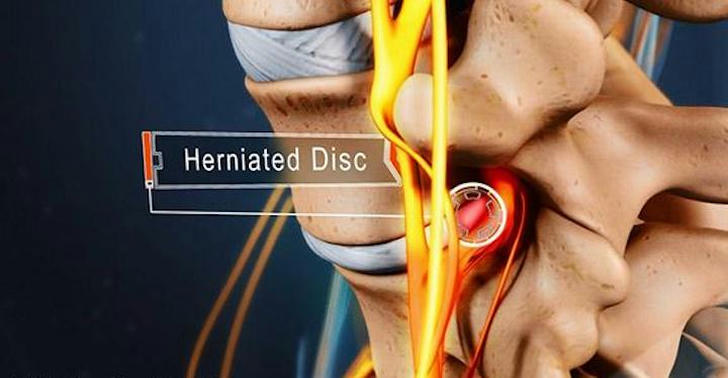
Lumbar disc herniation is a widespread condition affecting millions globally, often causing significant lower back pain and nerve-related symptoms. If left unrecognized or untreated, it can severely impact daily activities and overall quality of life. This article explores the risk factors, clinical signs, and diagnostic methods to help individuals identify early warning signs and take proactive measures.
📌 1. Epidemiology and High-Risk Groups of Lumbar Disc Herniation
| Aspect | Details |
|---|---|
| Prevalence | Affects ~5.5% of the global population; symptomatic disc degeneration impacts 400M+ people |
| Lifetime Risk | Estimated around 30%, with 1-3% experiencing symptomatic episodes |
| Demographics | More common in men aged 30–50; male-to-female ratio ~2:1 |
| High-Risk Occupations | Surgeons, professional athletes, drivers—jobs involving heavy lifting or repetitive strain |
| Genetic Influence | Strong hereditary factors contribute to disc degeneration |
| Lifestyle Factors | Smoking and increased visceral fat increase susceptibility |
🔹 Key Insight: Understanding these risk factors helps identify individuals who should adopt preventive strategies to reduce their risk.
📌 2. Recognizing Typical Symptoms and Clinical Manifestations
Primary Symptom: Localized low back pain in the lumbosacral region.
Pain Radiation: Unilateral pain radiating down buttocks and legs along nerve dermatomes.
Aggravating Factors: Sitting, squatting, exertion; relieved by rest.
Radicular Symptoms: Numbness, tingling, muscle weakness affecting mobility.
Pain Triggers: Standing, walking, coughing, sneezing intensify symptoms.
Additional Signs: Sensory loss and muscle weakness in affected limbs.
Assessment Tools: Pain and disability scales to evaluate intensity and life impact.
Differential Diagnosis: Important to distinguish from facet joint syndrome and discogenic pain.
🔹 Clinical Tip: Early recognition of these signs is crucial for timely intervention.
📌 3. Physical Examination and Clinical Tests for Accurate Assessment
| Test / Examination | Purpose & Interpretation |
|---|---|
| Muscle Strength Testing | Uses Medical Research Council scale to assess motor function |
| Sensory Disturbance Check | Identifies areas of numbness or altered sensation |
| Sphincter Function Test | Detects severe nerve involvement |
| Straight Leg Raise (Lasegue Test) | Positive result indicates nerve root irritation due to herniation |
| Crossed Straight Leg Raise | Confirms nerve root compression when positive |
| Other Tests (Bragard, Slump) | Limited evidence; not routinely recommended |
🔹 Diagnostic Approach: Combining multiple clinical signs (dermatomal pain, sensory deficits, motor weakness) improves diagnostic confidence.
📌 4. The Essential Role of Imaging in Diagnosis
| Imaging Modality | Features & Use |
|---|---|
| Magnetic Resonance Imaging (MRI) | Gold standard; non-invasive soft tissue visualization; detects disc displacement and nerve compression |
| Timing for MRI | Recommended after 6 weeks of symptoms or earlier if neurological deficits appear |
| MRI Findings | High T2 signal intensity in posterior disc region suggests herniation |
| Accuracy | Sensitivity and specificity up to 97% |
| Alternatives | CT and CT myelography valuable when MRI contraindicated or inconclusive |
| X-rays | Adjunct tool to exclude other lumbar pathologies |
| Advanced MRI Techniques | Includes grading systems and tractography for enhanced diagnosis and prognosis |
🔹 Imaging Insight: Accurate imaging is vital for confirming diagnosis and guiding treatment planning.
📌 5. Prevention and Management Strategies: From Lifestyle to Professional Care
| Strategy | Description |
|---|---|
| Modifiable Risk Factors | Smoking cessation, weight management to reduce abdominal fat |
| Activity Modification | Avoid strenuous physical tasks that strain the lower back |
| Posture & Exercise | Maintain proper posture; regular low-impact exercises to strengthen spinal support muscles |
| Conservative Treatment | Effective in 60–90% cases; includes physical therapy and NSAIDs for pain relief |
| Surgical Options | Microdiscectomy or disc replacement for severe or refractory cases |
| Early Diagnosis Importance | Combining lifestyle changes and medical care offers best outcomes |
🔹 Takeaway: A comprehensive approach integrating prevention and treatment preserves spinal function and quality of life.
🌟 Summary
Lumbar disc herniation is a common condition influenced by genetic, environmental, and lifestyle factors. Recognizing symptoms, conducting targeted physical exams, and utilizing advanced imaging enable accurate diagnosis. Prevention and management require a multifaceted strategy to reduce risks and apply appropriate treatments, ensuring optimal back health and life quality.
